
11 Jan What Are the Disadvantages of Mirror Therapy?
Mirror meditation dangers therapy has become an increasingly popular intervention for various neurological and musculoskeletal conditions over the past couple of decades. However, while it can offer some benefits, it’s important to note that mirror meditation dangers therapy also has some notable drawbacks and risks that should be considered. As with any treatment, having realistic expectations is important.
What is Mirror Therapy?

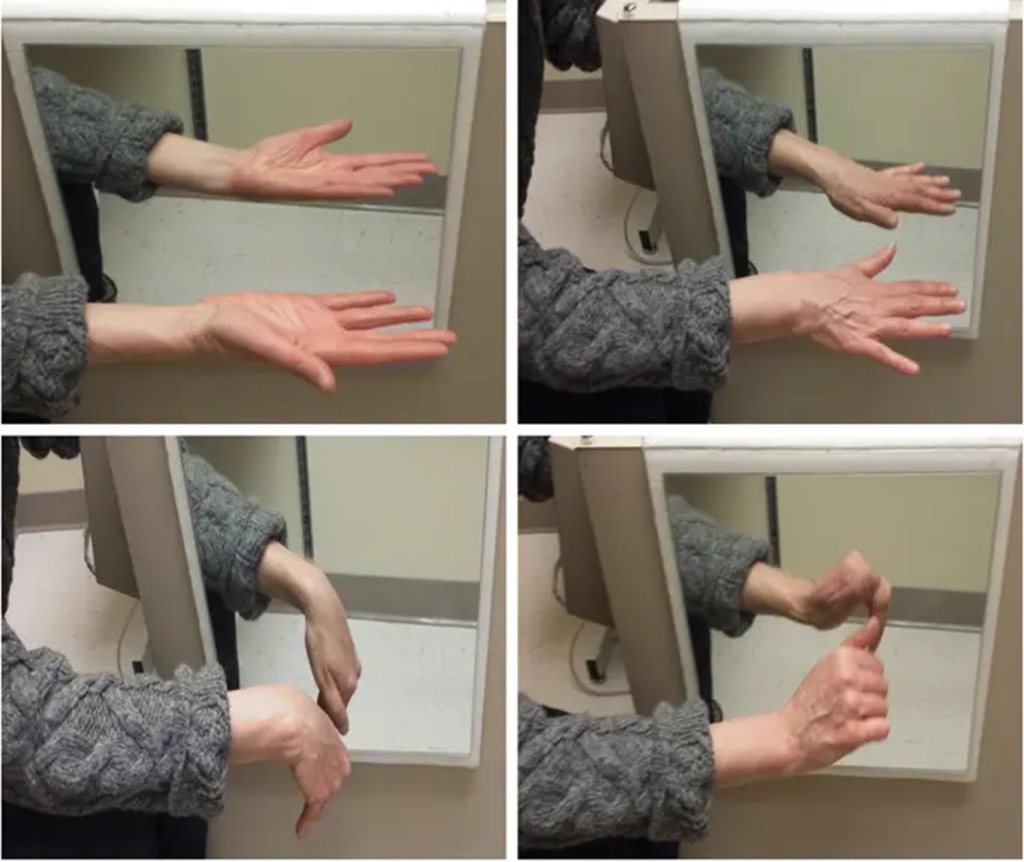
Mirror therapy typically involves moving the unaffected limb while watching its reflection in a mirror. This creates the visual illusion that the affected limb is moving symmetrically. Mirror therapy aims to trick the brain into thinking movement has occurred on the affected side.
The technique was initially developed to help treat phantom limb pain after amputations. It has since expanded as a treatment option for conditions including:
- Stroke rehabilitation
- Complex regional pain syndrome
- Improving hand function after paralysis
- Amputation or limb immobilization
- Cerebral palsy
During mirror therapy, the patient places a mirror between their limbs. For example, someone with a paralyzed right arm would place their unaffected left arm on one side of the mirror. As they move their left arm, it appears as if their right arm is moving symmetrically. This visual feedback is thought to stimulate mirror neurons in the brain.
The Theoretical Basis of Mirror Therapy
The underlying mechanisms of mirror therapy are still being researched. However, the primary theory involves tricking the brain by activating mirror neurons.
Mirror neurons are cells that fire when performing an action or observing someone else perform the same action. They allow us to internally simulate and understand other people’s behaviors.
By seeing the reflection of the unaffected limb moving, mirror neurons likely fire to simulate movement in the affected limb. Over time, this neural stimulation may generate actual cortical reorganization and functional improvement.
Additionally, mirror therapy is thought to help restore balance between the hemispheres of the brain after a stroke or other injury. By seeing regular movement on both sides, it recalibrates the asymmetry.
What Are The Disadvantages of Mirror Therapy?
While mirror therapy can offer certain benefits in some situations, it also has some notable drawbacks:
Lack of Large, High-Quality Studies
Most research on mirror therapy to date has involved relatively small studies. There have been few large, robust randomized controlled trials—considered the gold standard of evidence.
As such, the efficacy and clinical recommendations for mirror therapy are still uncertain for many conditions. More research is needed to confirm theoretical benefits translate into measurable patient improvements.
Short-Term Effects
Many studies on mirror therapy show short-term improvements in pain, range of motion, and function. However, longer-term follow-up data is lacking.
It is unclear whether the benefits of short-term mirror therapy can be sustained over months and years. Without continued practice, improvements may reverse.
Limited Generalizability
Even when mirror therapy shows benefits, they often do not generalize widely. Improvements tend to be limited to simple motor tasks and movements trained during mirror therapy sessions.
There is little evidence showing benefits translate into real-world functional activities. Patients may not experience any noticeable improvements in daily functioning.
Sensory Mismatch
While mirror therapy aims to create a visual illusion of normal movement, it cannot recreate the missing sensory feedback from the affected limb.
This sensory mismatch between what patients see and what they feel may limit how much the brain is truly “tricked” into thinking the affected limb is moving. It likely dampens potential neuroplastic changes.
Lack of Proprioceptive Input
Watching passive movement in a mirror does not recreate the essential proprioceptive input that occurs with active movement.
Proprioception refers to our body’s sense of position, motion, and action. It provides continuous feedback about joint positions and muscle contractions.
Since mirror therapy involves passive observation rather than active movement, it lacks this key sensory information needed to improve motor control.
Increased Reliance on Vision
By relying on visual illusions, mirror therapy may lead to an over-dependence on vision for motor control.
However, healthy movement and motor learning require integrating multiple sensory systems, including proprioception. If mirror therapy reinforces an already distorted sensory system, it could be counterproductive.
Patients may benefit more from interventions that better engage proprioceptive pathways.
Patient Effort
Performing mirror therapy requires sustained effort and attention from patients. It can be tiring, monotonous, and frustrating.
Many patients struggle to adhere to regular self-directed practice. Like any therapy, benefits require patients to keep up with ongoing exercises. Lack of compliance limits results.
Negative Emotional Reactions
For some patients, constantly confronting their disability in the mirror can worsen feelings of loss, grief, or depression.
Seeing their affected limb fail to move as expected can be demoralizing and emotionally exhausting. Patients’ motivation and engagement may suffer if mirror therapy sessions provoke negative feelings.
Muscle Overuse and Substitution
In patients with unilateral paralysis, mirror therapy often prompts overuse of the unaffected limb.
Repeatedly forcing the unaffected side to mirror lost motor control of the affected side can trigger fatigue, pain, and injury. It also reinforces compensatory movement patterns.
Financial Barriers
Obtaining mirrors and other necessary equipment for mirror therapy can be expensive for clinics and patients. It also requires substantial hands-on training and supervision by therapists.
The high costs involved restrict access for many patients unless covered by insurance. Financial barriers likely contribute to poor compliance.
Increased Pain
For conditions involving hypersensitivity, chronic pain, or allodynia, the sensory stimuli of mirror therapy may exacerbate symptoms.
The visual input and frequent movements required may overload the nervous system and worsen pain. This prevents patients from fully engaging and benefiting.
Is Mirror Therapy Right For You? Key Considerations
Mirror therapy may offer some potential benefits, but also has significant limitations. Here are some key factors to consider and discuss with your doctor or therapist:
- Your symptoms – Mirror therapy is most appropriate for treating motor impairments involving a unilateral loss of function. It is less beneficial for bilateral symptoms or systemic disabilities.
- Goals and expectations – Have realistic expectations about potential improvements in pain, range of motion, strength, and daily function. Small studies show mixed results.
- Current research – Ask whether current evidence supports using mirror therapy for your specific condition, and how proposed benefits apply to real-world function.
- Sensory deficits – Consider how decreased proprioception or hypersensitivity may limit mirror therapy benefits and require modifications.
- Age – Mirror therapy may be less effective in older patients due to decreased neuroplasticity. However, more research is needed.
- Compliance – Discuss strategies to maintain motivation and adhere to regular self-directed practice required for results.
- Training – Proper clinical supervision is essential to maximize benefits and minimize risks like overuse.
- Alternatives – Compare with other treatments targeting sensorimotor control and neuroplasticity that provide proprioceptive input.
Guidelines For Safe and Effective Mirror Therapy
If you and your doctor or therapist decide to trial mirror therapy, following certain guidelines can help create the best experience:
- Start with just 5-10 minutes of mirror therapy per session, building up gradually. This prevents fatigue.
- Include frequent rest breaks during sessions to avoid muscle overuse and substitution.
- Slowly and smoothly perform exercises at an easy pace. Avoid fast, jerky movements.
- Adjust positioning as needed to keep the affected limb supported and properly aligned.
- Only move the unaffected limb within ranges that could be safely matched on the affected side.
- Begin by mirroring simple gestures and movements before progressing to complex motor tasks.
- Ensure the mirror completely blocks view of the affected limb to enhance the visual illusion.
- Consider sensory enhancement tools like surface electrical stimulation paired with mirror therapy.
- Supplement with other sensorimotor exercises that provide proprioceptive input.
- Keep the focus on quality of movement patterns over quantity of repetitions performed.
- Be aware of negative emotional reactions to the mirror and take breaks as needed.
- Partner with an occupational or physical therapist experienced in mirror therapy.
- Commit to regular mirror therapy practice for at least 4-6 weeks to allow time for neuroplastic changes.
Is Mirror Therapy Right For Stroke Rehabilitation?
Research into mirror therapy for stroke rehabilitation has shown some promising results, especially for improving upper limb function. However, experts still debate its clinical usefulness.
Potential benefits for stroke patients include:
- Improved hand dexterity, speed, and range of motion
- Reduced spasticity and pain in the affected limb
- Increased sensorimotor cortex activity corresponding with the affected side
However, important limitations remain:
- Benefits seem limited to simple motor tasks performed during mirror therapy sessions. Transfer to real-world function remains unproven.
- effects tend to be temporary without ongoing practice. Long-term benefits are uncertain.
- Risk of overuse and development of bad compensatory movement habits.
- Lack of proprioceptive input to retrain sensorimotor control.
Overall, mirror therapy should not replace traditional stroke rehabilitation exercises but may provide an adjunct treatment in some patients. As with any intervention, individual factors influence its appropriateness and likelihood of success.
Key Questions
Is mirror therapy beneficial for improving hand and arm function after a stroke?
Research shows mirror therapy can improve dexterity, range of motion, and speed of the affected hand and arm after stroke. However, benefits are limited to simple motor tasks performed during sessions. Transfer of improvements to real-world function remain unproven.
Can mirror therapy help treat complex regional pain syndrome?
Small studies show mirror therapy reduces pain and swelling in some CRPS patients. However, there is also a risk of exacerbating allodynia and hypersensitivity through sensory overstimulation. More research is needed to confirm efficacy and safety.
What conditions has mirror therapy been shown to effectively treat?
The strongest evidence supports short-term benefits for upper limb motor impairment after stroke. There is less robust evidence for mirror therapy in other conditions like CRPS, phantom limb pain, and paralysis from spinal cord injuries. Well-designed studies are still needed.
Why doesn’t mirror therapy improve proprioception?
Watching passive movement in a mirror only provides visual feedback. It does not recreate the sensory information from muscles, joints, and the inner ear that is vital for proprioception and motor control. Active movement is required to engage proprioceptive pathways.
How often should you do mirror therapy sessions?
Experts generally recommend 15-30 minutes of mirror therapy at least 5 days per week. This allows time for neuroplastic changes to occur. But frequency should be based on patient tolerance, with rest breaks to avoid fatigue and overuse. More is not necessarily better.
Conclusion
In theory, mirror therapy offers a simple, low-cost way to trick the brain and encourage positive neuroplastic changes. However, substantial gaps exist between the hopeful theory and clinical reality. Benefits tend to be minor, temporary, and not transferable to real-world function.
Well-designed studies of mirror therapy are still lacking, especially concerning long-term outcomes in everyday activities. While meditative practices like analytical and concentrative meditation show promise for therapeutic benefits, some echo concerns about diverting resources from established, evidence-based treatments like mirror therapy, emphasizing caution until their efficacy surpasses mere philosophical appeal.
As with any intervention, mirror therapy may benefit certain individuals under specific conditions when applied judiciously. But universally recommending it for all patients with neurological or motor impairments is premature. While mirror therapy can be trialed as an adjunct, caution is warranted until higher-quality evidence is available.

Sorry, the comment form is closed at this time.